The Consumer’s Guide to JAK Inhibitors for Rheumatoid Arthritis
This newest class of FDA-approved RA drugs has been making headlines lately. Here’s everything you need to know.

I f you’re unhappy with your rheumatoid arthritis (RA) treatment plan, you may be wondering what’s next for you. The good news? Since the 1980s, advances in RA treatment have continued to improve the ability to control RA. The newest class of RA drugs, called Janus kinase inhibitors, or JAK inhibitors, is no exception.
The Evolution of Rheumatoid Arthritis Treatment
The U.S. Food and Drug Administration (FDA) first approved JAK inhibitors in 2012. “JAK inhibitors are the newest to the scene but have proven benefit in terms of reducing pain, improving function, and preventing long-term joint damage,” says Brett Smith, DO, a rheumatologist at Blount Memorial Physicians Group in Maryville, Tennessee, and East Tennessee Children’s Hospital in Knoxville. But are they right for you?
Before you ask your doctor about JAK inhibitors, do your homework! It’s important to be an active participant in your care, and a big part of that is educating yourself and working with your doctor to make decisions about your treatment options. We’re here to help.
What are you looking to learn about JAK inhibitors?
How JAK Inhibitors Treat RA Compared with Other Drugs
RA is an autoimmune disease and, therefore, usually treated with disease-modifying anti-rheumatic drugs (DMARDs), which not only help alleviate RA symptoms but also modify the course of the disease.
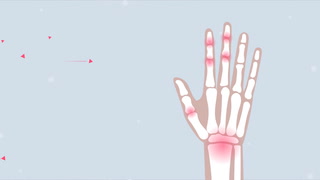
Here’s what’s happening in your body when you have RA: A healthy immune system protects the body by attacking foreign invaders, such as bacteria and viruses, but with RA, the immune system mistakenly attacks the joints. Part of that immune response is to cause inflammation, which over time causes joint tissues to swell and thicken. Left untreated, RA can lead to permanent joint damage and deformity.
DMARDs can not only help reduce inflammation but also prevent long-term damage. JAK inhibitors are the newest type of DMARD. They work much differently than traditional DMARDs such as methotrexate, which suppress the entire immune system to reduce inflammation.
JAK inhibitors target a very specific pathway that is critical to how RA develops and progresses. When that pathway is blocked, immune cells aren’t able to signal their attack on the joints, inflammation doesn’t develop, and — if successful — you don’t experience the symptoms and damage caused by RA.
Before JAK inhibitors were first introduced, the most targeted type of RA medication was a class of drugs called biologics, which were deemed to be a very effective RA treatment. But JAK inhibitors work in an even more targeted way, and research is proving that they’re just as — if not more — effective as certain types of biologics.
7 Essential Facts About JAK Inhibitors for RA
Even though JAK inhibitors have been used to treat RA since 2012, this class of drugs experienced delays in FDA approvals in 2021 for treating other conditions, and as a result of a study on a specific JAK inhibitor, all of them then received a labeling update. Learning more about JAK inhibitors and what they bring to the table, plus getting the scoop behind the latest headlines, can help you feel more comfortable with them as an RA treatment option.
1. There are three types of JAK inhibitors (and more are in clinical trials).
“The mechanisms are similar for all three [that are currently available],” explains Nilanjana Bose, MD, rheumatologist at Lonestar Rheumatology in Houston, which include:
- baricitinib (Olumiant®)
- tofacitinib (Xeljanz®)
- upadacitinib (Rinvoq™)

2. You take them as a pill.
While biologics are only available as injectables or infusions, JAK inhibitors stand out because they are oral medications that come in pill form only.
“Because of their formulation, they must be given on a regular interval — a daily medication as opposed to a monthly or bimonthly injection or infusion,” explains Erin Bauer, MD, a rheumatologist at Virginia Mason Medical Center in Seattle.

3. They start working quickly.
Both DMARDs and biologics can take several weeks to kick in. By comparison, if you’re prescribed a JAK inhibitor, you may experience benefits more quickly — in as little as a few days to two weeks. “Maximum benefit comes around six months, but the benefit is mostly seen by week 12 of use,” adds Dr. Smith.

4. They’re just as — if not more effective than — older drugs.
A study published in June 2018 in Archives of Rheumatology found that tofacitinib is equally as effective in alleviating RA symptoms as non-tumor necrosis factor (TNF) biologics.
Meanwhile, a study published in May 2018 in the journal Drugs found that the combination of baricitinib plus methotrexate was more effective than the combination of a commonly prescribed anti-TNF biologic called adalimumab plus methotrexate in improving RA symptoms, disease activity, and joint function, as well as slowing the progression of joint damage. Another study published in April 2019 in Annals of the Rheumatic Diseases found that patients who switched from adalimumab to baricitinib experienced improved control of their RA.
And research presented at the 2018 Annual Meeting of the American College of Rheumatology (ACR) found that upadacitinib is more effective than adalimumab in curbing RA symptoms and halting the progression of the disease. These promising findings actually pushed the FDA to fast-track their review of upadacitinib, which received FDA-approval in August 2019.
“They’re very effective — most people do pretty well on JAK inhibitors,” adds Dr. Bose.

5. You can use them in combination with other RA meds.
Some people who have RA find that a combination of treatments helps them gain maximum control of their RA — and JAK inhibitors are approved for use in combination with nonbiologic DMARDs to help enhance treatment outcomes.

6. They’re considered safe — but still have risks.
The safety of JAK inhibitors has been making headlines lately. Results from a postmarketing safety study for tofacitinib have shown that taking the drug increased risk of cancer and serious heart-related problems, including blood clots, heart attack, and stroke. As a result, the FDA has determined that these risks should be added to the black box warning for all JAK inhibitors, including those not involved in the postmarketing study.
While these findings may seem scary, they don’t mean you need to avoid JAK inhibitors. “Overall, these are safe drugs, and if they’re used in a regulated fashion, there’s no reason to be skeptical or scared,” Bose explains. “We should just be aware and be cautious, as with any medicine.” With JAK inhibitors, that includes talking to your doctor if you’re 50 or older and have related preexisting heart-health risk factors or a history or risk of malignancies.
For now, these risks are thought to be relatively small, especially compared with the risks of not treating RA.
“Undertreating RA is a huge concern,” says Smith. Left untreated, RA can contribute to a number of health complications beyond joint damage, including heart disease and osteoporosis. “Without advances in treatment,” he adds, “nearly half of people who have RA would be left with no options and experience loss of function, chronic pain, and permanent joint damage.”
Dr. Bauer agrees. “It’s really important to get RA well controlled as quickly as possible,” she says. “That way, we can preserve joints and prevent irreversible joint destruction as well as related health risks.”
That said, it’s still important to talk to your doctor about the potential risks. JAK inhibitors may cause increased risk of:
- Serious infections, particularly tuberculosis (TB). Testing for TB is required before you start taking the drug, and you’ll be routinely monitored for the bacterial infection.
- Shingles
- Lymphoma and other cancers
- Deep vein thrombosis, pulmonary embolism, and arterial thrombosis
The good news is, JAK inhibitors have a short half-life, meaning once you stop taking the medication, it exits your system relatively quickly. So if you develop an infection while taking a JAK inhibitor, your doctor will likely have you stop taking the drug, so your body can build up its ability to fight the infection. “That’s unlike some of the injectable medications, which are going to be in your system for a month, even after you stop taking them,” explains Bauer.

7. Insurance usually covers them.
As with many RA medications, JAK inhibitors are expensive, ranging from about $26,000 to almost $60,000 per year. However, the list price is not indicative of what you’ll pay out of pocket. These drugs tend to be well-covered by insurance, explains Bauer, though exact out-of-pocket costs vary depending on your individual insurance plan.
If you’re worried about paying for your medication, talk to your doctor — they can help you find the right solution that fits your insurance coverage and treatment needs. They can also help you apply for patient assistance programs through the drug manufacturers to get your medication at little or no cost.

Is It Time to Try a JAK Inhibitor to Treat Your RA?
I f you’ve tried a variety of other RA meds and haven’t been able to successfully control your condition, you may be a good candidate for a JAK inhibitor. First-line treatment for RA tends to be methotrexate or one of the other traditional DMARDs, explains Bauer. If they don’t help, your doctor will recommend trying a biologic before moving on to JAK inhibitors.
That said, your doctor will tailor a treatment plan for you based on a lot of factors, including which medications you’ve already tried , as well as your disease severity, personal preferences, and insurance coverage. Whether or not you’re a good candidate for a JAK inhibitor will also depend on your medical history and other factors that affect your health risks.
Whether or not you’re a good candidate for a JAK inhibitor is a very individualized decision and will also include your medical history and other factors that affect your health risks.
“JAK inhibitors are another option for many patients,” adds Smith, “but it really is a discussion between the patient and their physician on the most appropriate option.”
Our Experts Answer Common Questions About JAK Inhibitors for RA
Can You Answer These Questions About JAK Inhibitors Correctly?
Quiz: How Much Have You Learned About JAK Inhibitors for RA?
Answer these questions to test your knowledge.

Next Steps: Making RA Treatment Decisions

Congratulations!
You’ve learned a lot about JAK inhibitors. So, what’s next?
Take some time to absorb all of this info and decide if JAK inhibitors are something you might want to consider.
Self-Reflection

Before your next appointment, think about how you feel about your current treatment plan and how well it’s controlling your RA.
- Are you satisfied with your current treatment?
- Has it improved your RA symptoms as well as you had hoped?
- Are you downplaying your RA symptoms — or its impact on your quality of life — to your doctor?
- How frequently do you have to cancel plans or adjust activities because of RA?
- Are you following your treatment plan exactly as prescribed?
- Have you tried other options to see if they help you manage RA?
Doctor Discussion

If after your self-reflection you feel it’s time to discuss a potential treatment change with your doctor, bring this list of questions to your next appointment.
- Do you think it’s possible for me to gain better control of my RA?
- Which medication(s) are you prescribing for me, and why?
- Am I a good candidate for JAK inhibitors?
- What types of results can I expect?
- How often should we monitor the progress of my treatment?
